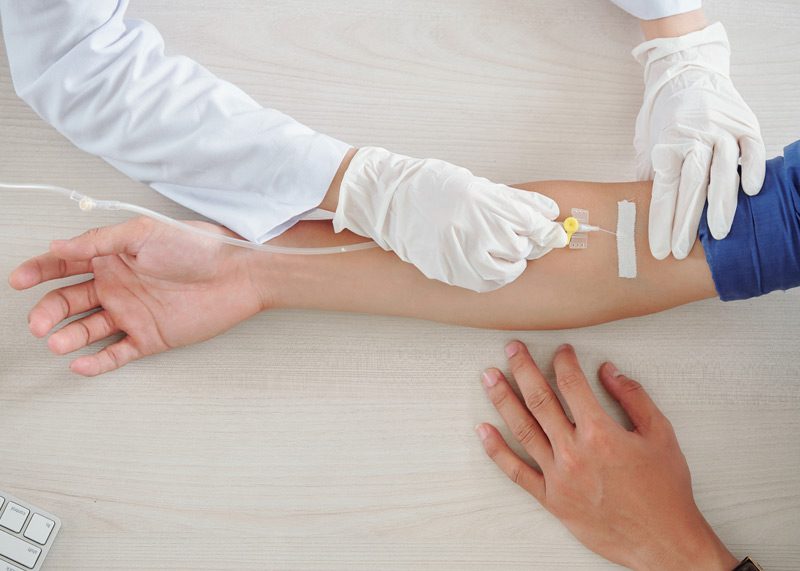

Intravenous (IV) therapy, or IV infusion, is a method of administering medicine or fluids directly into a vein to treat a range of medical conditions. During the infusion, a needle or catheter (tube) is inserted into the vein.
Conditions Treated With IV Therapy
Patients diagnosed with the following conditions may need IV therapy:
- Dehydration (loss of body fluids and inability to adequately hydrate)
- Malnutrition (nutrient deficiencies)
- Drug or alcohol dependence
- Cancer (to provide chemotherapy)
- Autoimmune disorders (the immune system mistakenly attacks the body’s own tissues)
- Infections and other diseases
Patients may need IV therapy if they’re unable to take oral medications or if the medication they need isn’t available in an oral form.
Some medication starts working faster and is more effective when administered directly to the bloodstream. An IV also provides greater control over the pace of medication delivery. For some situations, a PICC line may be used in order to administer medication or liquid nutrition for an extended period of time.

Types of IV Therapy
The four types of IV therapy are:
- IV line: The medication is administered directly into a vein using a needle.
- Central venous catheter and port: A tube is attached to a port under the patient’s skin.
- Central venous catheter: A tube is inserted into a vein in the chest.
- Peripherally inserted central catheter (PICC): A long tube is inserted through a vein in the arm that travels to larger veins near the heart.
IV Therapy Locations
Intravenous therapy may be provided in the following clinical settings:
- Hospitals
- Outpatient clinics
- Infusion centers
- Urgent care clinics
- Physician’s offices
Some patients may receive IV therapy at home. A visiting nurse or other healthcare provider from Active Plus Home Health Care, Inc. may administer the IV therapy in the patient’s home or teach them how to do it.
What to Expect During Intravenous Therapy
IV therapy is typically performed by a nurse or other trained healthcare professional. However, some patients may receive training to learn how to administer the IV therapy themselves. Or, a caregiver or loved one may provide IV therapy.
To begin IV therapy, a healthcare professional will attach a small tube into a vein in the patient’s arm. The small tube will be connected to an IV bag containing fluids or liquid medications. The IV fluid will travel into the bloodstream through a vein. The IV line will be attached to an automated pump or adjustable valve.
The patient will be monitored during the treatment to ensure the needle stays inserted, and the IV solution is flowing properly.
The entire process can take 30 minutes or longer, depending on the type of IV fluids or medication being administered. Once the patient has received all of the fluid or medication, the healthcare professional will remove the needle from the patient’s arm.
PICC Line Care
A peripherally inserted central catheter (PICC) is a long, thin tube (approximately 24 inches long) that is inserted into a vein in the arm and passed through to larger veins near the heart to deliver medication or liquid nutrition. On rare occasions, a PICC line may be placed in the leg. It requires careful monitoring for complications.
To avoid complications with a PICC line, a nurse will take the following steps and precautions:
- Replace torn or wet bandages.
- Avoid putting lotions or ointments under the dressing.
- Always wash hands with soap and water or use an alcohol-based sanitizer before and after handling the PICC line.
- Keep a smooth edge clamp on hand in case the tubing breaks.
- Follow doctor’s orders for flushing the line with saline or heparin.
- Ensure the clamps stay closed when not in use and when the cap is off.
- Use an alcohol cover to protect the end caps.
The dressing should be changed every three to seven days, or as directed by a healthcare professional. The dressing should also be changed if it becomes wet, dirty, or moves out of place. The nurse will check the patient’s skin every day for signs of infection, such as pain, swelling, redness, and oozing.